Post 37. A Face Moulded by Science, Softened by Care
The start of two years of wearing a perspex splint, a pioneering NHS specialist, and the compassionate lineage I never knew I was part of.
The clear plastic splint I wore on my face for two years was, by some distance, the hardest part of my medical recovery outside of my relentless operational schedule. It was uncomfortable, isolating, and at times, soul-sapping. But I endured it as I knew how crucial this treatment was and after a while, it became a part of me.
This isn’t a post about the emotional toll just yet. That comes next week and in other future posts. Today, I want to share how that splint came to be—and more importantly, the man behind it: Mr Mark Cutler.
It was incredible to re-connect and spend the morning with Mark recently
Scar tissue doesn’t just tighten; it rises. Our faces are our calling card to the world, so we had to act fast once Mr Clarke had finished patching up my face (for then). To stop the rising, pressure must be applied—relentlessly, strategically, and over time. For me, the answer was a prosthetic perspex face splint, custom-moulded (multiple iterations) to my changing face, worn 24 hours a day for two years.
If I wasn’t already unapproachable or “hard to look at” before, I certainly was now.
But as with many things in my recovery, the difference between enduring and embracing came down to information—and Mark was the one who gave it.
Dr Mark Cutler, my maxillofacial prosthetist, was a calm, open, motorbike-riding, rugby-playing genius. While Mr Clarke (my surgeon) was brilliant and formidable, Mark brought a different energy into the room. Emotionally intelligent, curious, and kind, he had this way of making the exceptional feel normal.
He was a pioneer too. Recently, while digging through notes for this project, I learned he was awarded the Fellowship of the Institute of Maxillofacial Prosthetists & Technologists in 1992—the same year I began treatment with him. He would later receive an MBE for his contributions to the field. Mum and I could already tell he was destined for that kind of recognition.
It’s just like going to the dentist really.
We spent hours in his clinic. I couldn’t talk during the face-moulding process, so he talked with Mum—and in doing so, supported her as much as he supported me. They built a rapport that gave her strength. Those hours in the chair, silent and still with warm wax and plaster being layered over my face, became strangely grounding. I breathed through straws, listened to Mark’s stories about weaving through traffic on his way into work from Gravesend, and waited to be peeled free like jelly from a mould.
Mark didn’t just fit me for a splint. He fit me into a lineage—one I only recently came to understand.
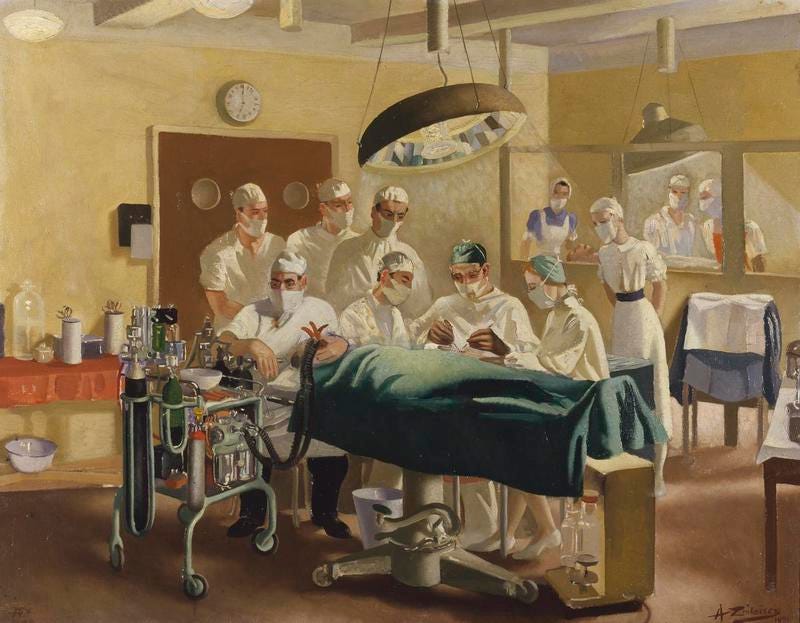
McIndoe operating at East Grinstead: painting by Anna Zinkeisen, 1944 (source)
Queen Victoria Hospital in East Grinstead, where Mark is now based (and where I tracked him down), was home to the Guinea Pig Club—an informal group of WWII pilots who became early recipients of pioneering plastic surgery. They were treated by Sir Archibald McIndoe, who didn’t know how to graft or dress burns at first but experimented until he found what worked. They called themselves guinea pigs because that’s how it felt.
The unbreakable spirit of these chaps (source)
Mark picked up that same spirit of innovation. The materials used for my splint—modern polymers like PET (Polyethylene terephthalate)—came into the field largely by accident. A food packaging supplier mentioned the material to him, and Mark chased it down. He eventually sourced it from a Glasgow-based company and began experimenting on me and two others. “Wow,” he recalled for me recently, “it was so much better than anything we’d used before.”
He added:
“We knew how bad things got [for patients’ faces] when we couldn’t apply pressure properly. And then you came along—and it wasn’t happening to you guys with this new material. That was a win.”
Previously tried plastics were either too thick and rigid or too brittle. And the idea of having to wear a pressure garment-style hood or balaclava for years—let’s not go there.
My old friend. As soon as I picked it up I immediately knew this was an updated and lighter version than I would’ve worn. If my accident had happened a little earlier, I’d have been wearing something akin to below - no thank you!
He laughed at how far things have come since.
“Back then, I poured goop all over your face. Now, we’d just scan you and 3D print it.”
But the new tech wasn’t the only thing that made the experience bearable. It was Mark himself.
He wore one of the splints himself for six months—just to understand what it would feel like for his patients. I only found this out when we reconnected and it blew me away. He didn’t do it for pity’s sake—but to deliver better, more compassionate care.
Mark knew words mattered, too.
“We never called it a mask,” he told me. “Too many negative connotations. We called it a facial splint. Especially with younger patients, you need to take them by the hand. You don’t say, ‘Here’s what you’ve got to wear.’ You create trust.”
And he did. Not just with me, but with my mum, too. His gentleness made her feel like she wasn’t alone. Like we were in good hands. And we were.
So many patients’ (mostly suffering cancer) lives have been massively improved at the hands of Mark and his colleagues.
I had two types of splints. One I could talk through and eat with during the day—held on my head with a big strap and by little elastic bands and fitted with a removable mouthpiece. The other was a solid one-piece I wore at night. It locked my jaw in place and took ages to get used to. Mum said it broke her heart every evening to help remove the day splint, cream my face, and “lock me up” for the night.
But we did it. Because Mark had given us the why. And with the why, we could endure almost anything.
There’s one more quote from Mark I want to leave you with:
“You’re like a role model. You are remarkable. Society still has a problem with disfigurement—but to have powerful, positive, objective people like you is quite rare in our world.”
The more I get into my own story, the more I’m able to see the things that truly made the difference. To have had multiple world-leading pioneers (you haven’t been introduced to them all yet) under one hospital roof caring for me was ridiculous. But they all offered more than just technical skill—they were ahead of their time when it came to compassionate care, too.
Mark may have thought he was just doing his job. But Mark, you changed my life—and helped me become the kind of person who is not just trying, but capable of being, a role model.
Next week, I’ll write about how this splint-wearing boy edged back into society. But for now, I want to honour the man—and the lineage—that made it possible.